Deadline Extended for EEO-1 Filing from March to May 31, 2019
It’s Time to Take (Rural) Matters into Your Own Hands!
President Trump Says Vote on GOP Health Care Plan to Come After 2020 Election
BLS Data on Worker Access to Family Leave in 2018 Now Available
Compliance Strategies for Workplace Wellness
Deadline Extended for EEO-1 Filing from March to May 31, 2019
The Equal Employment Opportunity Commission (EEOC) has extended the deadline for employers to submit EEO-1 Reports for 2018. The reports are now due by May 31, 2019.

What is the EEO-1 Report?
The EEO-1 Report is a federally mandated survey that collects workforce data from employers. The data is categorized by race, ethnicity, sex and job category. The EEOC uses this information to enforce federal prohibitions against employment discrimination and discriminatory pay practices.
The EEO-1 Report is an annual survey required under Title VII of the federal Civil Rights Act (Title VII). Under the law, employers with 100 or more employees and certain federal contractors must use the EEO-1 Online Filing System to submit employment data by March 31 every year. The EEOC extended the 2019 deadline because the federal government shutdown delayed the online system’s opening for 2018 reports. The EEOC expects the system to become available for 2018 submissions in early March 2019.
What’s Next?
Employers should monitor the EEO-1 website for more information about EEO-1 filing requirements and about when the filing system will be open for 2018 Reports. In the meantime, employers filing EEO-1 Reports for the first time should register to receive a company login, password and further instructions from the EEOC.
If the preparation or filing of an EEO-1 Report would create undue hardship, an employer may send a written request for an exemption or for special reporting procedures to the EEOC. Employers may also obtain a one-time, 30-day extension of the EEO-1 filing deadline by emailing a request to the EEOC.
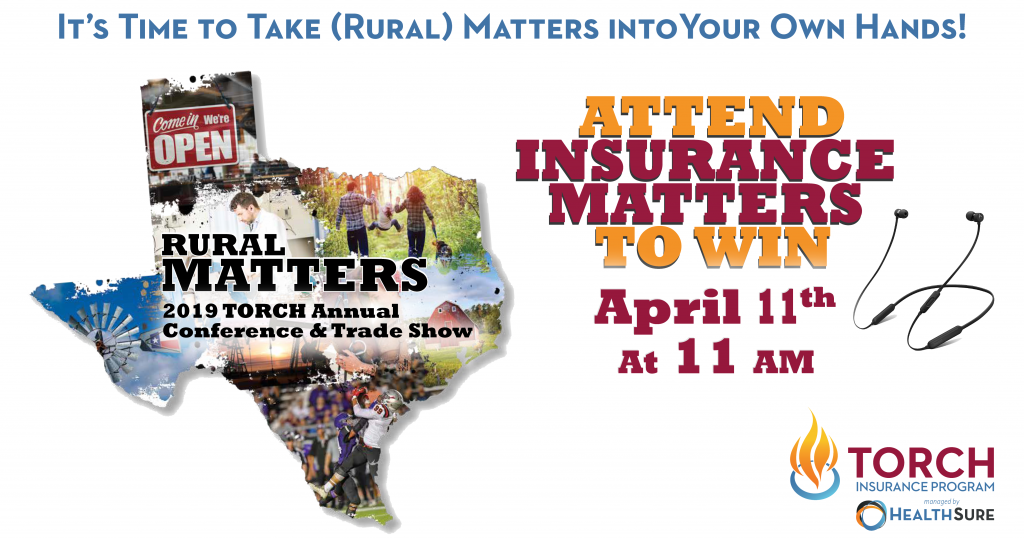 A panel of experts will be discussing the strategies in this article during a breakout facilitated by HealthSure at the TORCH Annual Conference & Trade Show from April 10 to 12 at the Hyatt Regency in Dallas.
A panel of experts will be discussing the strategies in this article during a breakout facilitated by HealthSure at the TORCH Annual Conference & Trade Show from April 10 to 12 at the Hyatt Regency in Dallas.
If you want to know if any or all of these strategies are right for your hospital, and the practical steps you can take to get started, be sure to include our workshop in your conference plans. (It’s at 11 a.m. on April 11th).
There are also recorded webinars on these and other topics available on the RHIA website. You can find them here.
President Trump Says Vote on GOP Health Care Plan to Come After 2020 Election
On Monday, April 1, 2019, President Donald Trump stated in a series of tweets that a vote on a Republican Party (GOP) replacement health care plan for the Affordable Care Act (ACA) won’t take place until after the 2020 elections.
GOP’s Health Care Plan
President Trump’s tweets stated that the ACA’s deductibles and premiums are “far too high” and that a replacement is needed. He continued to state that the GOP’s replacement plan for the ACA will have “far lower premiums (cost) [and] deductibles” and will be “much more usable.” He also affirmed that the GOP’s plan would support those with pre-existing conditions.
These tweets came one week after the president directed the Department of Justice (DOJ) to support a federal court ruling that the ACA is unconstitutional.
DOJ Support of Court Ruling Invalidating the ACA
On March 25, 2019, the DOJ filed a letter with the 5th Circuit Court of Appeals agreeing with the lower court’s Dec. 14, 2018, ruling in Texas v. Azar. This means that the DOJ believes the lower court’s ruling should stand, and the ACA should be struck down as unconstitutional due to the elimination of the individual mandate in 2019.
What does all of this mean for employers and employees?
While the recent developments may seem like major health care change is on the horizon, employers and employees can expect things to remain the same for the time being.
The court ruling invalidating the ACA is currently being appealed, and industry experts anticipate that the Supreme Court will likely take up the case, meaning that a final decision won’t be seen until then.
As such, all existing ACA provisions will continue to be applicable and enforced. Although the individual mandate penalty will be reduced to zero beginning in 2019, employers and individuals must continue to comply with all other applicable ACA requirements.
BLS Data on Worker Access to Family Leave in 2018 Now Available
The Bureau of Labor Statistics (BLS) recently released a The Economics Daily (TED) report on civilian access to paid and unpaid family leave in 2018. These statistics provide insight into family leave benefits trends across the country. For this report, family leave included leave to care for family members, maternity and paternity leave.
Paid Family Leave Access
In March 2018, 16 percent of workers in the private sector and 17 percent of civilian workers had access to paid family leave. In the public sector, 25 percent of state and local government workers had access to this type of leave. Leave access varied by the size f the employer.
Unpaid Family Leave Access
In March 2018, 89 percent of civilian workers and 88 percent of private sector employees had access to unpaid family leave. Ninety-four percent of state and local government workers had access to this type of leave. As with paid family leave, access to leave varied by employer size.
For access to the BLS data, click here.
Compliance Strategies for Workplace Wellness
Workplace wellness programs have many benefits, but employers must carefully design them to comply with several federal laws. Recent developments have created new compliance challenges for 2019.
It is important to keep the following in mind when designing your workplace wellness program:
Only individuals who participate in the GHP are eligible for the wellness plan.
The GHP’s summary plan description should describe the wellness plan.
Individuals who elect COBRA for the GHP are eligible to continue the wellness plan. As such, it should be included in GHP COBRA notices.
The wellness program collects personal health information that must be protected.


