TRUE GRIT ISSUE
Georgia “Lone Ranger” Finds Friends in Texas
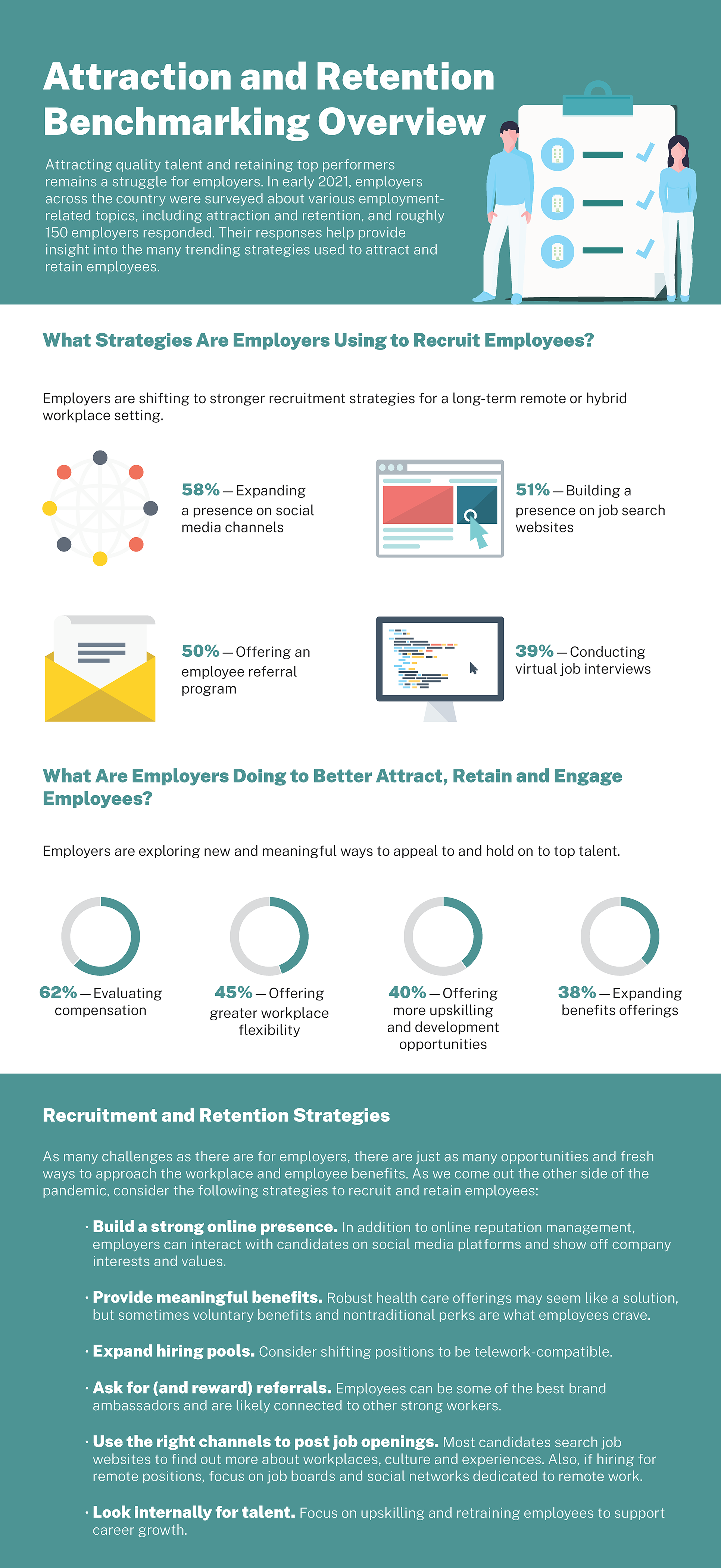
2021 EBHR Survey – Attraction and Retention Benchmarking Overview
U.S. Supreme Court Rejects ACA Challenge
The Economics of Perseverance
By Brant Couch, CIC, CPA
The science of economics is the study of human behavior; it examines the decisions we make around utilizing resources to achieve our goals. For leaders of rural and community hospitals, finding new ways to succeed, despite having to cope with perennially scarce resources, requires no small amount of perseverance and grit.
Psychologist Angela Duckworth, in her best-selling book Grit: The Power of Passion and Perseverance, says it isn’t intelligence, talent or skill, but resolve and perseverance – grit – that makes people successful.
The economics of perseverance, as I see it, has two parts: the decisions we make, and the outcomes we achieve, when constantly confronted with scarcity.
Decisions, decisions, decisions
When it comes to decision making, psychologists say the brain has a very limited cognitive capacity (the total amount of information we can remember at any given moment). For example, if you ask a person to remember seven digits they will need to use at the end of the day, their brain will basically be full until they no longer have to remember those seven digits. Imagine how full our brains are when we constantly worry about scarcity.
Preoccupation with scarcity affects our confidence, limits our ability to find solutions to problems, causes us to neglect other priorities, and can lead to some very poor decisions. Psychologists call the limiting effects of a scarcity mindset “tunneling”. In my work with hospital leaders, I often see the damage tunneling causes.
Scarcity-driven tunneling occurs when we are consumed with managing short-term needs, and it affects how hospital leaders decide to use financial and physical resources. When hospital leaders spending most of their, energy and brain power on dealing with surviving it seems impossible to look long term on how their hospital can thrive.
Leaders who persevere are those who decide to not let scarcity consume all their time, energy, and brain power. They decide to spend some of it on the longer term. They stay open to new ideas, constantly seek the help of others, and explore new opportunities within their hospitals, communities and among their peers.
The law of collaboration
The law of supply and demand is a foundational economic principle constantly at work in today’s rural and community hospitals. It is a little simplistic to say it this way, but the demand for income and funding – for money – always seems to be greater than the supply. On any given day, protecting the sources of money already in place is what hospital leaders worry about the most. As necessary as it is, focusing on protecting the money can lead to scarcity-driven tunneling.
On the other hand, a foundational principle of the economics of perseverance says that when demand outstrips supply, you need to look around for new supply sources while reducing – or at the least, taking greater control of – demand.
How do you crawl out of the scarcity tunnel when you are in it all alone and there is no light at either end? Sadly… you don’t, you’re stuck.
But, like dozens of rural hospitals leaders have discovered, there is a way out. It is called the law of collaboration and it’s another foundational principle of the economics of perseverance.
The law of collaboration states that the magnitude of a challenge is inversely proportional to the amount of collaboration. In simpler terms: the more you collaborate, the easier it is to overcome challenges.
Talk about outcomes!
Some recent examples of the outcomes caused by collaboration include the Community Hospital Insurance Coalition (CHIC), two forms of direct contracting, and an innovative approach to managed care contracting.

All four have helped rural hospital leaders find new or grow existing income (supply). Three of the four have had a direct positive impact on their ability to control cost (demand).
I have written extensively about CHIC but, in a nutshell, it’s a medical stop-loss reinsurance program made possible by the collaboration of 24 (and counting) rural hospitals. CHIC emerged from a collaborative entity called Rural Hospital Insurance of America (RHIA). Over 80 rural and community hospitals participate in RHIA in pursuit of its mission.
As CHIC succeeds through its fourth year, we project participants will have shared a total of approximately $3 million in distributions. That is new money that comes from owning your insurance instead of renting it… something that would not be possible without the collaboration of like-minded hospital leaders.
On the demand side, CHIC has empowered participating hospital leaders and their teams to achieve greater cost control through purposeful, data-driven wellness initiatives and employee education programs. Simply said, hospital employees now know they have skin in the game and are doing their part to protect their health and be wiser consumers of healthcare. Plus, by pooling their buying power, CHIC participants receive preferred services and pricing from the various vendors they engage collectively.
Contracting for dollars
More recently, we have seen a significant increase in direct contracting to control hospital employee healthcare cost (demand) and increase income from regional employers (supply). By directly contracting with tertiary hospitals, rural hospital leaders are gaining greater control of employee healthcare costs by negotiating agreements where mutual interest exists. This has cleared a path for better communication, both between the hospitals and with employees. And, as you can imagine, a path for better control of costs when employees need care at a tertiary hospital.
By negotiating agreements with regional employers, hospital leaders have been able to retain existing and attract new patients. By collaborating with employers, hospital leaders are creating win/win relationships. The hospital gets more money while the employer gets greater control of their healthcare spend.
Managed care contracting is not new but, thanks to the collective buying power and shared wisdom of many hospital leaders, significant improvements are being found with the resulting contract renegotiation favoring the rural hospital.
It takes a village
…to protect rural healthcare in America.

When scarcity is allowed to dominate our thinking and our lives, it is natural to hunker down in our personal tunnel of expediency. But, think about this, the strategies I have described in this article are succeeding because of collaboration. Hospital leaders who embrace the economics of perseverance are committed supporters of state and federal associations.
The good news is through RHIA we collaborate with hospitals nationwide. As well as with partners like TORCH (Texas Organization of Rural & Community Hospitals), National Rural Health Association, and other groups across the country that are keepers of the rural healthcare flame and catalysts for greater collaboration.
Scarcity is not likely to ever go away and it is largely out of our control. On the contrary, refusing to be oppressed by scarcity is a choice we can all make. By collaborating directly with each other, and by participating in and supporting our state and national associations, we all benefit from the economics of perseverance.
Please feel free to contact me with your comments, questions and collaborative ideas.
Brant Couch is the CEO of HealthSure
HealthSure manages the Rural Hospital Insurance of America program (RHIA) in collaboration with the National Rural Health Association (NRHA). It is the insurance program manager for the Texas Organization of Rural and Community Hospitals (TORCH). And, the insurance program manager for the New Mexico Rural Hospital Network (NMRHN).
Georgia “Lone Ranger” Finds Friends in Texas
Gritty CEO adds CHIC to impressive winning resume
By Heidi Hughes
Angela Ammons, CEO of Clinch Memorial Hospital in Homerville, GA knows a lot about perseverance and grit. Despite family circumstances that left her practically homeless at age 15, she had the grit to find work, take care of herself, get a college degree on her own, climb the ranks from doctor’s receptionist to nursing staff supervisor and then into her first CEO position.

Long story short:
- When Angela became CEO In September of 2017, Clinch Memorial had just recorded its ninth consecutive money-losing year and it only had enough cash on hand for a few more days of operations and making payroll seemed impossible.
- Today, the hospital is thriving and Ammons and her team have been recognized across the state and nationally for their accomplishments. (For a more detailed account of Angela’s journey, read this Time Magazine article.)
Recently Clinch Memorial joined 25 other hospitals collaborating in an initiative called the Community Hospital Insurance Coalition (CHIC). HealthSure’s Heidi Hughes sat down with Angela to discuss what was behind her decision to join CHIC.
Heidi: Why did you decide to go from a fully-insured employee benefits plan to owning part of an insurance captive like CHIC?
Angela: “We had the state health benefit plan but it did not help me because I could not have a hands-on approach for helping my employees become healthier.
Going from paying a premium to writing a check up to our stop loss limit was really scary for me. But I could not drive or encourage my staff to use our own facility… everyone was using CVS, Lab Core… they were going to competing physicians instead of our own primary care physician.
The only way I could get a grasp on that, and to help them, was to develop a program that was better tailored for us specifically. I mean, why would any healthcare facility not have a policy that says, ‘OK guys, if we do that here, you have to get it done here.’ Why would you not do that? You cannot do that with the state health benefit plan or with Blue Cross, Blue Shield.
Plus, I like the idea that when we perform well, we get a little prize* at the end of the year that goes back in our coffers.”
Heidi: CHIC is a national program but Clinch is the first hospital in Georgia. What helped you decide to join?
Angela: “Well, it’s still nerve racking. Some nights I sit up and think, ‘What have I done!’
Being a lone ranger in Georgia was a little bit terrifying at first but I definitely had validation going to the TORCH conference. (TORCH is the Texas Organization of Rural and Community Hospitals. Angela attended and met several CEOs whose hospitals also participate in CHIC.) Speaking with the participants that have been in this initiative, there was not one complaint. They all just said, ‘We should have done this a million years ago!’
It’s like finding that miracle drug or – I hate to even say this – it’s like that day you decide to leave that horrible relationship. You’re like ‘Oh my God, I should have done this 10 years ago!’”
Heidi: In terms of how the program works, were there any parts that you struggled with during your decision-making?
Angela: “I was worried about our initial financial responsibility. But I felt better after they (HealthSure) did an evaluation of our current health plan usage and are very honest about what our out of pocket would be if we didn’t change.
They were very up front about what we would be putting into the captive and after I saw that it just made it a no brainer.”
Heidi: The health of your staff – in addition to the financial health of your hospital – is a major concern for you. What has happened in this regard since you joined CHIC?
Angela: “I started having mandatory meetings because I realized my staff was not fully understanding their part. I said something like, ‘Guys, you have to understand that when you get a CT scan at a competing hospital, I am writing a check to the competing hospital. At the end of the day that means your bonuses, your raises. But, if we do really well as a health system, next year I plan on decreasing your deductibles and giving you a little more benefit. I cannot pass that along to you as long as you are not using this health plan as appropriately as you should.’
They all walked away with their eyes wide open and fully understanding their part… I’m hoping it will just get better and better.”
Heidi: Central to our work is making sure rural and community hospital CEOs never go it alone. CHIC was created by Rural Hospital Insurance of America (RHIA), a national entity, powered by the National Rural Health Association (NRHA) and managed by HealthSure with over 80 participating hospitals. Now that you are part of this group, what do you look forward to?
Angela: “It’s simple. I cannot see why I would not want to join a captive of rural hospitals that have already done this and done it well. I can benchmark our performance against theirs.
When we win, we all win. And, even if we don’t do so great, guess what, there are well performing members of the team who pick us up. No state plan is going to do that. There is no other self-insured plan that is going to do that.”
*As it enters its fourth year, it is estimated CHIC hospitals will have shared $3 million or more in dividends.
U.S. Supreme Court Rejects ACA Challenge