Contents
ACA Litigation May Affect Employers
ACA Litigation May Affect Employers
A New York district court will hear the first case on whether employers may reduce their employees’ work hours in order to avoid providing health benefits required under the Affordable Care Act (ACA).

The case is Marin v. Dave & Busters-a class action lawsuit claiming that the restaurant chain, Dave & Busters, violated federal law by intentionally interfering with its employees’ eligibility for health benefits.
The ACA requires applicable large employers (ALEs) to offer affordable, minimum value health insurance coverage to their full-time employees, or to pay a penalty. For this purpose, a “full-time employee” is defined as an employee that works, on average, at least 30 hours of service per week. In addition, Section 510 of the Employee Retirement Income Security Act (ERISA) prohibits employers and
plan sponsors from interfering with an
employee’s rights to health benefits under the plan.
According to the group of about 10,000 employees who filed suit, their hours were significantly reduced for the purpose of keeping them below the ACA’s “full-time employee” threshold.
On Feb. 9, 2016, the court rejected Dave & Busters’ motion to dismiss the case. This is the first case of its kind, and will set a precedent for other employers who are considering or have implemented similar strategies regarding their employees’ work hours as a result of the ACA.
On Feb. 29, 2016, the Department of Health and Human Services (HHS) released its final Notice of Benefit and Payment Parameters for 2017. For 2017, the rule increases the ACA’s out-of-pocket maximum to $7,150 for self-only coverage and $14,300 for family coverage.
The rule sets individual coverage open enrollment periods for these benefit years:
- 2017: Nov. 1, 2016 to Jan. 31, 2017
- 2018: Nov. 1, 2017 to Jan. 31, 2018
- 2019 and beyond: Nov. 1 to Dec. 15 of the prior year
The rule also creates a new Exchange model for state-based Exchanges using the federal platform and establishes six standard plan options in the individual federal Exchanges.
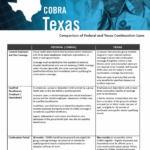
The federal and state guidelines regarding federal COBRA requirements and the Texas continuation laws can seem complex. Click here for a comparison of federal COBRA requirements and Texas continuation coverage laws. It should help simplify the complex issue so you can be sure to stay in compliance.
The growing utilization of private exchanges could prove to be a game changer for health care. According to a recent Kaiser Family Foundation report, about 2.5 million people were enrolled through private exchanges in 2014, including about 1.7 million group plan enrollees, 700,000 individual Medicare enrollees and 100,000 individual enrollees.
The employers that are shifting employees to private exchanges tend to be in lower-wage industries. Still, many of the exchange platforms surveyed anticipated significant growth in the future across industry lines. This trend could be related to continued employer cost control.
The information provided in this alert is not, is not intended to be, and shall not be construed to be, either the provision of legal advice or an offer to provide legal services, nor does it necessarily reflect the opinions of the agency, our lawyers or our clients. This is not legal advice. No client-lawyer relationship between you and our lawyers is or may be created by your use of this information. Rather, the content is intended as a general overview of the subject matter covered. HealthSure and Marathas Barrow Weatherhead Lent LLP are not obligated to provide updates on the information presented herein. Those reading this alert are encouraged to seek direct counsel on legal questions.


