Gag Clause Attestation
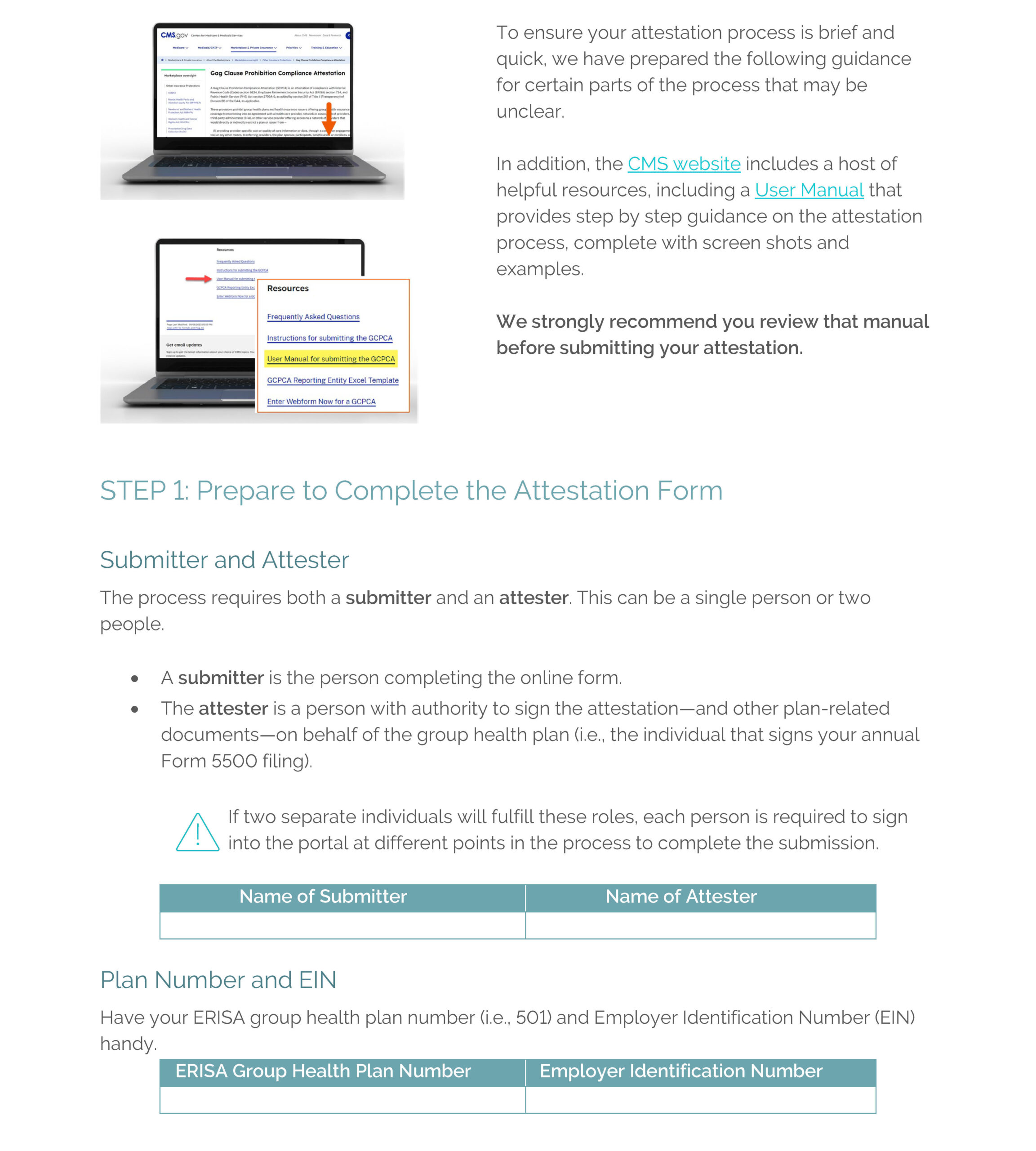
Deadline for Submitting Gag Clause Attestation Is Dec. 31, 2023
Agencies Issue Additional FAQs Regarding the Transparency in Coverage Final Rules
On September 27, 2023, the DOL, IRS, and HHS released FAQs About Affordable Care Act Implementation Part 61 (“FAQ Part 61”) which addresses lingering questions about enforcement of the Transparency in Coverage Final Rules (TiC Final Rules), specifically the provisions of the TiC final rules requiring plans and carriers to post machine-readable files for in-network negotiated rates and historical net prices for all covered prescription drugs by plan or issuer at the pharmacy location level (“Rx rates”), and the status of a previously announced enforcement safe harbor applicable to in-network (“INN”) provider rates for covered items and services which allowed plans with percentage-of-billed-amount contracts or other alternative reimbursement arrangements to report this information differently if the dollar amount could not be determined in advance.
If you recall, the TiC Final Rules required non-grandfathered group health plans (other than those consisting of excepted benefits or account-based plans) to make available to the public three separate machine readable files (“MRFs”) including detailed pricing information related to (1) negotiated rates for all covered items and services between the plan or issuer and in-network providers (“INN provider rates”), (2) historical payments to, and billed charges from, OON providers (“OON allowed amounts”), and (3) the Rx rates.
Beginning on July 1, 2022, machine readable files for INN provider rates and OON allowed amounts were required to be posted by plans; however, in Q1 of FAQs About Affordable Care Act Implementation Part 49 released by the agencies in August of 2021 (“FAQ Part 49”), the agencies delayed the requirement to release Rx rates machine readable files as they evaluated whether the requirement would be duplicative of other transparency and reporting obligations related to prescription drugs, specifically the RxDC reporting required under the Consolidated Appropriations Act of 2021 (“CAA”). In FAQ Part 61, the agencies report that, after reviewing the Rx DC reporting results, they have determined “there is no meaningful conflict between the reporting requirements” under the RxDC reporting and the TiC Rx rates machine readable file requirement as the CAA requires disclosure of different and additional information than required in the TiC Final Rules.
Therefore, the agencies have rescinded Q1 of FAQ part 49 and intend to develop technical guidance and an implementation timeline for plans to post their Rx rates machine readable files. Thus, the machine readable files for prescription drugs will be due once that technical guidance and timeline are released. This does not impact the requirement for plans to continually update (on a monthly basis) their machine readable files for the OON allowed amounts and INN rates for covered items and services.
FAQ Part 61 also addresses another enforcement safe harbor, which was previously announced in FAQs About Affordable Care Act Implementation Part 53 (“FAQ Part 53”) released by the agencies in April 2022, which applied to INN provider rate MRFs for plans with alternative reimbursement arrangements (such as reference-based pricing) or percentage of billed charges contracts. Under FAQ Part 53, the agencies indicated that where contractual arrangements are for a percentage of the billed charge or use a different, alternative funding arrangement, then plans were to use the applicable percentage in the rate box or the open text box to describe the nature of the negotiated rate, respectively.
FAQ Part 61 clarifies that the agency did not intend to apply a “categorical exception” to this reporting requirement. Whether a plan can comply with the requirement to provide a specific dollar amount is a facts and circumstances test and a safe harbor only applies in circumstances where a plan can demonstrate it is extremely difficult or impossible for a plan or issuer to determine and report a rate for a specific item or service (for the reasons specified in FAQ Part 53). In these instances, plans may continue to follow the technical guidance on GitHub.
Conclusion
No action with regard to the prescription drug machine readable files is required right now. The FAQ was essentially a “heads up” from the agencies indicating that they will request this reporting be completed, but they intend to provide guidance and some lead time after the guidance is issued for plans to post the files. We will release another update once the technical guidance and timeline are released. In the meantime, plans must continue to update their INN rates and OON allowed amount machine readable files monthly.
Plans with percentage of billed charges contracts or other alternative reimbursement arrangements should consult with counsel to review the FAQ and TiC Final Rules in light of their funding arrangement to determine whether they may still be able to use the standard set forth in Q2 of FAQ Part 61 (i.e., that they can demonstrate it is extremely difficult or impossible to determine and report a rate for a specific item or service) for their INN rate machine readable files, and to ensure they understand whether there is any risk in doing so.
The IRS has released final 2023 forms and instructions for reporting under Internal Revenue Code Sections 6055 and 6056:
- 2023 Forms 1094-B and 1095-B (and instructions) will be used by providers of minimum essential coverage, including self-insured plan sponsors that are not applicable large employers (ALEs), to report under Section 6055.
- 2023 Forms 1094-C and 1095-C (and instructions) will be used by ALEs to report under Section 6056, as well as for combined Section 6055 and 6056 reporting by ALEs who sponsor self-insured plans.


